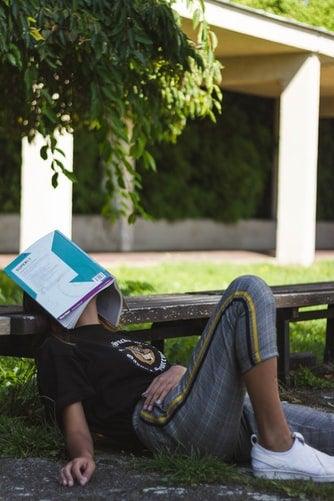
Your child daydreams a lot at school and is easily distracted when they are doing homework or chores. Maybe they fidget constantly. You might wonder if they have attention-deficit/hyperactivity disorder (ADHD). Or is it attention deficit disorder (ADD)?
Is there a difference?
Many people use the terms to mean the same thing -- and that's sometimes correct. But not always.
ADD is a type of ADHD that doesn't involve constant movement and fidgeting. But it's a blurry distinction. The confusion dates to 1994. That's when doctors decided all forms of attention-deficit disorder would be called "attention-deficit/hyperactivity disorder," even if the person wasn't hyperactive. Now it's called ADHD, inattentive type, or ADHD, hyperactive/impulsive type, or ADHD, combined type.
Which term is right for your family to use depends on your child's specific symptoms and diagnosis. It's important to talk with an experienced mental health provider to make sure your child gets the right diagnosis.
Daydreamer or Fidgeter?
ADHD is a brain-based disorder. It can interfere with your child's everyday activities at home and at school. Kids who have it have trouble paying attention and controlling their behavior, and are sometimes hyperactive.
Before they are diagnosed, you will want to note your child's symptoms. The CDC offers an ADHD checklist for children that may help you keep track of them.
Here are the signs to look for:
- Inattention: Includes disorganization, problems staying on task, constant daydreaming, and not paying attention when spoken to directly.
- Impulsivity: Includes spur-of-the-moment decisions without thinking about the chance of harm or long-term effects. They act quickly to get an immediate reward. They may regularly interrupt teachers, friends, and family.
- Hyperactivity: Involves squirming, fidgeting, tapping, talking, and constant movement, especially in situations where it's not appropriate.
Mental health professionals in the United States use the Diagnostic and Statistical Manual of Mental Disorders (DSM) to diagnose all psychiatric conditions, including ADHD. The latest version divides it into three types:
- ADHD predominantly inattentive presentation (what used to be called ADD)
- ADHD predominantly hyperactive-impulsive presentation
- ADHD combined presentation
ADHD Predominantly Inattentive Presentation (ADD)
Kids with this condition aren't hyperactive. They don't have the high energy level seen in others with ADHD. In fact, children with this form may seem shy or "in their own world."
ADD is diagnosed if a child under age 16 has 6 or more symptoms of inattention (5 or more for older teens) for at least 6 consecutive months but no signs of hyperactivity/impulsivity.
The symptoms include:
- Trouble paying attention (easily sidetracked)
- Doesn't like or avoids long mental tasks (such as homework)
- Trouble staying on task during school, at home, or even at play
- Disorganized and seems forgetful
- Doesn't appear to listen when directly spoken to
- Doesn't pay close attention to details
- Loses things often
- Makes careless mistakes
- Struggles to follow through with instructions
Children with this subtype of ADHD may go undiagnosed because the symptoms may be chalked up to daydreaming.
ADHD Predominantly Hyperactive-Impulsive Presentation
Children with this form of ADHD have tons of energy and are constantly moving in a way that causes problems. It's diagnosed if a child under age 16 has 6 or more hyperactive/impulsive symptoms for at least 6 months (5 or more for older teens). This form is more noticeable than the inattentive type.
Symptoms include:
- Blurting out answers before a question is finished
- Constantly interrupting others
- Trouble waiting for their turn
- Talks too much
- Fidgeting, tapping, and squirming
- Gets up when it's not appropriate (such as when the teacher is talking or in the middle of dinner)
- Running or climbing in inappropriate situations
- Unable to play quietly
- Always "on the go"
ADHD Combined Presentation
A child with this type has symptoms of both inattention and hyperactivity/impulsivity.